- MRSA-colonized patients who have been identified in a hospital by active surveillance culturing may not need to be isolated to prevent their bacteria being transmitted to other patients by healthcare workers — provided hospital staff and visitors adhere to very vigorous handwashing. (P. Wilson, University College Hospital, London; press release)
- An engineered coating made of titanium dioxide with added nitrogen could be employed as an antibacterial surface in hospitals; exposure to ordinary white light activates the compound to kill E. coli and may be useful against MRSA also. (Z. Aiken, UCL Eastman Dental Institute; press release)
- The natural antiseptics tea tree oil and silver nitrate enhance bacterial killing when combined, which may also allow them to be used in lower doses – important for avoiding toxicity. It may also be possible to deliver them encapsulated in engineered sphere made of lipids called liposomes. (W.L. Low, University of Wolverhampton; press release)
- Overuse of antibiotics in farming is not only breeding resistant bugs in animals, it is also changing soil ecology and depleting nitrogen-fixing bacteria that improve soil fertility. The antibiotics are affecting soil when manure from drug-using farms is spread as fertilizer. (H. Schmitt, University of Utrecht; press release)
Antibiotic resistance. The things we do to make it worse. And anything else I find interesting.
31 March 2009
MRSA news from Europe - Society for General Microbiology
The annual meeting of the UK's Society for General Microbiology is taking place this week, so here's a quick roundup of MRSA-related news. As with these posts from a year ago, abstracts are not online; in a few cases there are press releases from the science-news service EurekAlert.
29 March 2009
British newspaper discovers ST398, says no UK cases - incorrect
The UK's Sunday Express takes note today of "pig MRSA" ST398 (full post archive here) in a story that is both somewhat alarmist and oddly incomplete, since it misses a piece of news that I told you about here last June.
The Express story raises the alarm over ST 398 in pigs in the Netherlands, colonizing farmers and causing human illnesses. There is nothing in it that we have not already discussed here many times, but it is nevertheless worth noting because it appears to be the first report on ST398 in a year in a major UK paper. (Credit for what I think is the first mention of ST398 in the Brit press goes to the Independent.)
But here's what's odd about the story: It says (italics mine),
Credit for pushing the story of ST398 in the UK goes to the organic/sustainable farming group the Soil Association, who have aggressively monitored and lobbied for the extremely slow reveal of ST398 by the British government. As the issue now stands, the UK tested British pigs for ST398 colonization in 2008, but has not revealed the results. It has not yet tested retail meat in the UK, some of which is imported from the Netherlands, the location where the most ST398 has been found.
While that sounds like foot-dragging, it is still ahead of the US: Except for the study published in January by Tara Smith's team at University of Iowa (paper here, my Scientific American story here), there has been no testing of pigs in the US, certainly none by government agencies.
(Hat-tip to Pat Gardiner for alerting me to the Sunday Express article.)
The Express story raises the alarm over ST 398 in pigs in the Netherlands, colonizing farmers and causing human illnesses. There is nothing in it that we have not already discussed here many times, but it is nevertheless worth noting because it appears to be the first report on ST398 in a year in a major UK paper. (Credit for what I think is the first mention of ST398 in the Brit press goes to the Independent.)
But here's what's odd about the story: It says (italics mine),
A DEADLY new form of MRSA is believed to be spreading from farm animals to humans – already the bacteria has been found in hospitals abroad.However as constant readers here already know, ST398 has already has been found in UK hospitals: in three unrelated patients — one adult and two newborns — in a Scottish hospital, none of whom had any relationship to pig-farming.
It is the first time the bug has spread in this way and experts believe excessive use of antibiotics in factory-farmed animals may be behind its development.
“Farm animal” MRSA, as it is known, can cause a raft of illnesses including skin infections, pneumonia, bone infections and endocarditis. …
The new MRSA bug, known as ST398, could reach hospitals in the UK, causing serious illness and death among vulnerable patients. (Byline Lucy Johnstone and Martyn Halle)
Credit for pushing the story of ST398 in the UK goes to the organic/sustainable farming group the Soil Association, who have aggressively monitored and lobbied for the extremely slow reveal of ST398 by the British government. As the issue now stands, the UK tested British pigs for ST398 colonization in 2008, but has not revealed the results. It has not yet tested retail meat in the UK, some of which is imported from the Netherlands, the location where the most ST398 has been found.
While that sounds like foot-dragging, it is still ahead of the US: Except for the study published in January by Tara Smith's team at University of Iowa (paper here, my Scientific American story here), there has been no testing of pigs in the US, certainly none by government agencies.
(Hat-tip to Pat Gardiner for alerting me to the Sunday Express article.)
28 March 2009
Consumers Union: 18% of Americans have had a hospital infection in self or family
Constant readers: You may not be aware that Consumers Union (yes, the nonprofit that publishes the magazine Consumer Reports) has a marvelous project called Stop Hospital Infections that has been instrumental in pushing for hospital-infection reporting and MRSA-control laws, offering support to citizen activists who want change in their states and offering text of a model MRSA-control act. (Stop Hospital Infections is in the blogroll at right.)
They have just released a survey — of more than 2,000 U.S. adults, performed March 12-16, 2009 — that gives us an excellent, and very sobering, look at what is happening with hospital-acquired infections. The news is not good:
They have just released a survey — of more than 2,000 U.S. adults, performed March 12-16, 2009 — that gives us an excellent, and very sobering, look at what is happening with hospital-acquired infections. The news is not good:
- 18% reported that they or an immediate family member had acquired an infection owing to a hospital stay or other medical procedure.
- 61% of those who acquired an infection said it was "severe" and 35% characterized it as "life-threatening."
- The risk of an infection increased 45% if a patient spent the night in the hospital.
- 53% of Americans polled said these infections required additional out of pocket expenses to treat the infection.
- 69% had to be admitted to a hospital or extend their stay because of the infection.
27 March 2009
Germs: All-singing, all-dancing, all urging you to wash your hands
Because it is Friday, and we could all use a laugh... I'm currently writing about a hospital system that has had very good success with an institution-wide campaign to promote hand-washing.
The system is called Novant Health Care. They won a major award from the Joint Commission last year (months after I interviewed them, news-radar points to me). Their campaigns have worked so well that they have put their graphics (images for posters, computer wallpapers, wndow films and the like) free for download here.
But what was new to me is their hand-hygiene promoting video, which they have put on YouTube, featuring a singing, dancing E. coli channeling Barry Manilow. Ladies and gentlemen, I give you: Soapacabana.
(Wanders away, humming: My name is Germy, I like it dirty...)
The system is called Novant Health Care. They won a major award from the Joint Commission last year (months after I interviewed them, news-radar points to me). Their campaigns have worked so well that they have put their graphics (images for posters, computer wallpapers, wndow films and the like) free for download here.
But what was new to me is their hand-hygiene promoting video, which they have put on YouTube, featuring a singing, dancing E. coli channeling Barry Manilow. Ladies and gentlemen, I give you: Soapacabana.
(Wanders away, humming: My name is Germy, I like it dirty...)
26 March 2009
MRSA research at Society for Healthcare Epidemiology of America meeting
As promised, a round-up of some of the research presented at the annual meeting of the Society for Healthcare Epidemiology of America (SHEA), held last weekend in San Diego. (Disclosure: I was on the faculty for the meeting; in exchange for co-hosting a session, SHEA will be reimbursing me for airfare and hotel. I wasn't otherwise paid, though.) There were 143 presentations on MRSA; here are a few.
I'm going to put in links to the online abstracts — I have SHEA's permission to do this — but I can't guarantee how long they will stay up. For those outside the science world, what happens at these meetings is that research is presented, in slide/PowerPoint sessions or in a poster, as a preliminary step to getting it published in a journal. Once a journal expresses interest, a cone of silence descends, the researchers are asked not to discuss the research until the paper is printed, and the abstract will probably be taken offline.
So, efforts to control hospital MRSA are showing some success:
I'm going to put in links to the online abstracts — I have SHEA's permission to do this — but I can't guarantee how long they will stay up. For those outside the science world, what happens at these meetings is that research is presented, in slide/PowerPoint sessions or in a poster, as a preliminary step to getting it published in a journal. Once a journal expresses interest, a cone of silence descends, the researchers are asked not to discuss the research until the paper is printed, and the abstract will probably be taken offline.
So, efforts to control hospital MRSA are showing some success:
- Invasive hospital-onset MRSA infections declined 16% from 2005 to 2007, and hospital-associated community-onset infections went down almost 9% — probably, though not provably, because of in-hospital prevention campaigns. (A. Kallen et al.)
- MRSA control in a small ICU (22 beds) leads to MRSA reductions throughout a 270-bed Montana community hospital. (P.J. Chang et al.)
- Swabbing the nose and culturing the swab, the classic test to check for MRSA colonization, misses 30% of positive patients because they are colonized in the groin or armpit. (C. Crnich et al.)
- If a hospital does not use AST (active surveillance and testing, or "search and destroy") it may seriously underestimate its MRSA incidence, though it may be able to detect general trends. (P.J. Chang et al.)
- But medical centers of similar size and situation that did v. did not use AST achieved similar reductions in hospital infections. (K. Kirkland et al.)
- Most of the cases of MRSA colonization identified in a Delaware healthcare system were found so soon after admission that they must have begun out in the community and were not due to hospital transmission. (K. Riches et al.)
- The proportion of MRSA bloodstream infections caused by community strains (proven microbioogically) doubled at Chicago's main public hospital between 2000 and 2007. (K. Popovich et al.)
- One out of every 7 ICU cases of MRSA in Atlanta's major public hospital involved a community strain. (H. Blumberg et al.)
- The number of MRSA infections brought to a Chicago-area ER increased 566% between 2002 and 2007, and was seasonally clustered (D. Buchapalli et al.)
- Hospital-associated community-onset cases accounted for 58% of all invasive MRSA in the US between 2005 and 2007, with patients undergoing dialysis or those who have been in long-term care the most vulnerable. (J. Duffy et al.)
25 March 2009
Bill in Congress: "Preservation of Antibiotics for Medical Treatment" Act
Important news for anyone concerned about the spread of "pig MRSA" ST398: Rep. Louise Slaughter (D-NY) and Sen. Edward Kennedy (D-MA) have introduced a bill that would restrict important classes of antibiotics for use against disease only, taking them out of the realm of subtherapeutic use or growth promotion in agriculture. The bill would allow the use of the antibiotic classes for disease in animals as well as in humans; the intent is to preserve the drugs' effectiveness for as long as possible.
The text of the bill, the Preservation of Antibiotics for Medical Treatment Act of 2009, is here.
A Reuters story in which Slaughter predicts the bill will have a difficult time is here; she has introduced it several times in the past decade, but it has never made it through.
Support from the Pew Commission on Industrial Farm Animal Production is here. An earlier version was supported by the American Academy of Family Physicians here.
The National Pork Producers' Council's response is here.
(Hat tip to Barry Estabrook at Politics of the Plate and to Melinda Hemmelgarn, the FoodSleuth.)
The text of the bill, the Preservation of Antibiotics for Medical Treatment Act of 2009, is here.
A Reuters story in which Slaughter predicts the bill will have a difficult time is here; she has introduced it several times in the past decade, but it has never made it through.
Support from the Pew Commission on Industrial Farm Animal Production is here. An earlier version was supported by the American Academy of Family Physicians here.
The National Pork Producers' Council's response is here.
(Hat tip to Barry Estabrook at Politics of the Plate and to Melinda Hemmelgarn, the FoodSleuth.)
Kindle owners: My first book now available, with a MRSA chapter
It was news to me, until a friend of mine went and bought it: My first book, Beating Back the Devil: On the Front Lines with the Disease Detectives of the Epidemic Intelligence Service, has been put into a Kindle edition.
BBtD was the first and so far only book to go inside the CDC's "outbreak police." It tells a year in the life of the first class of young physicians and PhDs to join the Epidemic Intelligence Service after the anthrax attacks — the first year, in other words, in which the EIS officers knew in advance that the possibility of confronting bioterrorism was no longer hypothetical. It tracks members of the class around the planet, from West Nile virus to foodborne illness to malaria prevention in Malawi to SARS. In alternating chapters, it also tells the hidden history of the EIS, which was founded in 1951 as a post-Korean War force for bioterror detection. Its members were in on every major disease event of the second half of the 20th century: the launch and near-failure of the polio vaccine, the end of smallpox, the beginning of AIDS, and the emergency investigation of the anthrax attacks (during which I was embedded with a CDC team).
Most important for our purposes here, BBtD takes you inside an investigation of a MRSA outbreak — in Los Angeles in 2003, when gay men who frequented sex clubs began developing cripplingly serious skin infections, and a young CDC investigator had to determine whether to call on the city to shut the clubs down...
BBtD was the first and so far only book to go inside the CDC's "outbreak police." It tells a year in the life of the first class of young physicians and PhDs to join the Epidemic Intelligence Service after the anthrax attacks — the first year, in other words, in which the EIS officers knew in advance that the possibility of confronting bioterrorism was no longer hypothetical. It tracks members of the class around the planet, from West Nile virus to foodborne illness to malaria prevention in Malawi to SARS. In alternating chapters, it also tells the hidden history of the EIS, which was founded in 1951 as a post-Korean War force for bioterror detection. Its members were in on every major disease event of the second half of the 20th century: the launch and near-failure of the polio vaccine, the end of smallpox, the beginning of AIDS, and the emergency investigation of the anthrax attacks (during which I was embedded with a CDC team).
Most important for our purposes here, BBtD takes you inside an investigation of a MRSA outbreak — in Los Angeles in 2003, when gay men who frequented sex clubs began developing cripplingly serious skin infections, and a young CDC investigator had to determine whether to call on the city to shut the clubs down...
Ten tips for avoiding hospital infections
ScientificAmerican.com (disclosure: I have written a story for them, and it is edited by a friend) has a great interview with a hospital epidemiologist about things to do to avoid hospital infections.
It's a smart list, with some non-obvious things on it. For instance:
It's a smart list, with some non-obvious things on it. For instance:
5. Make sure you're kept warmThe whole list is worth reading.
The air temperature in operating rooms typically hovers between 65 and 69 degrees Fahrenheit (18 and 20 degrees Celsius). That's great for the doctors and nurses bundled head to toe in scrubs, but not necessarily for the person on the table. [Stephen Streed, an epidemiologist who oversees infection control at the Lee Memorial Health System in Fort Myers, Fla.] says that the body responds to chilly air by constricting vessels supplying blood to the skin and the tissues just below it; diverting blood away from the body's surface and toward its core is the body's strategy for conserving heat. With less blood supplying oxygen to the incision site, the immune cells there become oxygen-deprived and therefore less effective at battling invading germs. Ask the surgical team how they intend to keep you warm -- if they will crank up the room temperature by a few degrees, cover you in blankets, or warm you with IV fluids, for instance.
6. Ask about presurgery antibiotics
For many operations, including those involving the heart and bone, doctors routinely give patients preventive antibiotics to nip infections in the bud. One dose is typically given via IV an hour before the surgeons make the first cut, and sometimes two more doses are given over the next 24 hours, Streed says. If you think there is any possibility that you have an infection before going into surgery, tell your doctor so that he or she can treat you first. (Having an existing infection in, say, the bladder or skin ups the risk of developing a second, surgery-related infection, Streed warns.)
21 March 2009
More on "pig MRSA" and the havoc it can do
Folks, before I get to the SHEA abstracts, one more post on ST398 in humans, and a sad and difficult story. It is the first (to my knowledge) report of ST398 spreading into a nursing home, in the January 2009 issue of Eurosurveillance Weekly.
It was very thoroughly investigated, because it took place in the Netherlands, where by national policy there is active surveillance and testing — AKA "search and destroy" — for MRSA in health care facilities.
To me it is both an object lesson in the unpredictable spread of this newly recognized organism, and also an exploration of the deep human cost of combatting it.
The nursing home, in a town called Doorn, is described as a residence for "visually and intellectually disabled" people, and it sounds like a good place, made of 35 household-like units that hold 8 residents each, with a pretty high ration of staff to residents. One resident in one unit was an adult man (age not given) who was completely blind and significantly mentally disabled. Since 2004, he had been living with hidradenitis suppurativa, a condition of painful, recurring, weeping infections of the skin that can be caused by staph. Periodically, he was treated with a variety of antibiotics — tetracycline,erythromycin, flucloxacillin, trimethoprim/sulfamethoxazole, clindamycin, minocycline, rifampicin — but none of them seem to have made much difference to the infections. (Hidradenitis is an awful condition; there are times when the only treatment is skin grafts.)
In October 2007, the regular swabs taken of his infections suddenly showed not drug-sensitive staph, but MRSA. Confirmatory swabs showed that he was colonized with MRSA in the nose, throat and groin. After analyzing whom he might have been in contact with, the home identified 43 resident and staff at risk, swabbed them all, and found 2 other residents and 3 staff members colonized. That led to another round of swabbing, of 160 people, but no other cases of colonization were found.
So, just to recap, that is the index case, with MRSA infections and colonization in various places on his body, plus five others who were only colonized.
Sequencing/typing of the isolates found that all 6 were carrying ST398, falling into one of two spa types, t2383 and the more rare t011. None of the residents or staff had had any contact with livestock. They did have play/therapy animals at the residence — rabbits, chickens and goats — but they were checked and were all negative. The source was never found.
The five who were only colonized were given 5 days of decolonization therapy: mupirocin gel (Bactroban) in the nose and showers with chlorhexidine soap (Hibiclens). Afterward, they had to be proved negative on three successive nasal cultures; the paper does not say how far apart the cultures were. Until the third negative culture, staff had to stay home, and residents were banned from group activities. Underlining that: Physically or mentally disabled adults living in an enclosed, supportive society had to be isolated from it because they acquired this bug. Just think how difficult that must have been. The paper notes: "The outbreak caused commotion among the staff members, and they had a lot of practical questions as they were unfamiliar with MRSA and an MRSA-outbreak in particular. Furthermore, it turned out that the use of gloves, surgical masks and aprons during washing and clothing was perceived as threatening by the clients."
The index case's situation is even sadder. He was given a private bath and shower, and essentially restricted to there and to his private room. He had been in group day-care, but was switched to being minded by himself. His "social contacts with other residents who lived in other units was restricted to a minimum" — presumably he was not able to be fully secluded from the other members of his household. However, anyone who came into direct contact with him — for instance, to bathe and dress him — had to be on contact precautions: gloves, aprons and surgical masks. This went on for six months while his very refractory MRSA was treated with oral antibiotics and surgical incision and drainage of his abscesses; after six months, his symptoms had not resolved, but swabs of his wounds were MRSA-negative, and some of the isolation precautions were lifted.
Underlining: Someone blind and mentally disabled, presumably fairly secure in the enclosed, supportive society of the residential home, has to be restricted from his routine, from people who are probably his friends, and from all skin-to-skin contact, for half of a year.
Now, mind you: If you or I had a relative in that home, we might want them to do exactly what they did do. It is difficult to say how well the staff might have succeeded in getting mentally disabled residents to cooperate with, for instance, hand-washing.
But this is not the first case I have heard of where the cost of protecting a group from MRSA has fallen very, very hard on one individual. I am not going to argue with the Dutch policies, but in this case, I find their unintended consequences terribly sad.
It was very thoroughly investigated, because it took place in the Netherlands, where by national policy there is active surveillance and testing — AKA "search and destroy" — for MRSA in health care facilities.
To me it is both an object lesson in the unpredictable spread of this newly recognized organism, and also an exploration of the deep human cost of combatting it.
The nursing home, in a town called Doorn, is described as a residence for "visually and intellectually disabled" people, and it sounds like a good place, made of 35 household-like units that hold 8 residents each, with a pretty high ration of staff to residents. One resident in one unit was an adult man (age not given) who was completely blind and significantly mentally disabled. Since 2004, he had been living with hidradenitis suppurativa, a condition of painful, recurring, weeping infections of the skin that can be caused by staph. Periodically, he was treated with a variety of antibiotics — tetracycline,erythromycin, flucloxacillin, trimethoprim/sulfamethoxazole, clindamycin, minocycline, rifampicin — but none of them seem to have made much difference to the infections. (Hidradenitis is an awful condition; there are times when the only treatment is skin grafts.)
In October 2007, the regular swabs taken of his infections suddenly showed not drug-sensitive staph, but MRSA. Confirmatory swabs showed that he was colonized with MRSA in the nose, throat and groin. After analyzing whom he might have been in contact with, the home identified 43 resident and staff at risk, swabbed them all, and found 2 other residents and 3 staff members colonized. That led to another round of swabbing, of 160 people, but no other cases of colonization were found.
So, just to recap, that is the index case, with MRSA infections and colonization in various places on his body, plus five others who were only colonized.
Sequencing/typing of the isolates found that all 6 were carrying ST398, falling into one of two spa types, t2383 and the more rare t011. None of the residents or staff had had any contact with livestock. They did have play/therapy animals at the residence — rabbits, chickens and goats — but they were checked and were all negative. The source was never found.
The five who were only colonized were given 5 days of decolonization therapy: mupirocin gel (Bactroban) in the nose and showers with chlorhexidine soap (Hibiclens). Afterward, they had to be proved negative on three successive nasal cultures; the paper does not say how far apart the cultures were. Until the third negative culture, staff had to stay home, and residents were banned from group activities. Underlining that: Physically or mentally disabled adults living in an enclosed, supportive society had to be isolated from it because they acquired this bug. Just think how difficult that must have been. The paper notes: "The outbreak caused commotion among the staff members, and they had a lot of practical questions as they were unfamiliar with MRSA and an MRSA-outbreak in particular. Furthermore, it turned out that the use of gloves, surgical masks and aprons during washing and clothing was perceived as threatening by the clients."
The index case's situation is even sadder. He was given a private bath and shower, and essentially restricted to there and to his private room. He had been in group day-care, but was switched to being minded by himself. His "social contacts with other residents who lived in other units was restricted to a minimum" — presumably he was not able to be fully secluded from the other members of his household. However, anyone who came into direct contact with him — for instance, to bathe and dress him — had to be on contact precautions: gloves, aprons and surgical masks. This went on for six months while his very refractory MRSA was treated with oral antibiotics and surgical incision and drainage of his abscesses; after six months, his symptoms had not resolved, but swabs of his wounds were MRSA-negative, and some of the isolation precautions were lifted.
Underlining: Someone blind and mentally disabled, presumably fairly secure in the enclosed, supportive society of the residential home, has to be restricted from his routine, from people who are probably his friends, and from all skin-to-skin contact, for half of a year.
Now, mind you: If you or I had a relative in that home, we might want them to do exactly what they did do. It is difficult to say how well the staff might have succeeded in getting mentally disabled residents to cooperate with, for instance, hand-washing.
But this is not the first case I have heard of where the cost of protecting a group from MRSA has fallen very, very hard on one individual. I am not going to argue with the Dutch policies, but in this case, I find their unintended consequences terribly sad.
20 March 2009
"Sick as a pig" - from ST398
Constant readers, I am at the annual meeting of the Society for Healthcare Epidemiology of America, where there is a lot of news about MRSA in hospitals. I hope to post on that over the next few days.
In the meantime, though, I want to pass on several pieces of news about ST398, the "pig strain" that we have talked so much about.
First, the Soil Association, the British organic/sustainable farming group that has done much work elucidating the spread of ST398 and making the link between that bug and antibiotic use on farms, has released an online documentary about ST398 called Sick as a Pig. You can watch it here, and here is the Soil Association's press release:
In the meantime, though, I want to pass on several pieces of news about ST398, the "pig strain" that we have talked so much about.
First, the Soil Association, the British organic/sustainable farming group that has done much work elucidating the spread of ST398 and making the link between that bug and antibiotic use on farms, has released an online documentary about ST398 called Sick as a Pig. You can watch it here, and here is the Soil Association's press release:
...40% of Dutch pigs and up to 50% of Dutch pig farmers are now carrying the new strain, which is also spreading to the wider population. Although this type of MRSA was first detected in humans in the Netherlands as recently as 2003, it now causes almost one in three cases of MRSA treated in Dutch hospitals.Second, here is a paper from last fall that somehow slipped by me: in the CDC journal Emerging Infectious Diseases, a report of two cases of ST398 infection in men in Sweden. Neither had any contact with farming or animals.
It is not yet known whether any British pigs are affected by the new strain of MRSA (called ST398) since the results of testing, which was required by the EU and carried out in 2008, have not been made public.
Several countries have already published the results of their own tests revealing significant levels of MRSA in national pig herds. The European Food Safety Authority has said that, 'It seems likely that MRSA ST398 is widespread in the food animal population, most likely in all Member States with intensive animal production'.
The first patient, a previously healthy 36-year-old male physiotherapist, sought medical care in March 2006 for a small abscess in his axilla. Culture of the abscess grew MRSA. Presence of mecA gene was confirmed by PCR. During the next 2 months, furunculous [sic] developed twice, caused by the same strain. His youngest child, adopted from China, had been found to be MRSA positive (throat, perineum, and a small wound) a month earlier during routine screening for adopted children. During subsequent screening of the family, the older sister, adopted from South Korea, was also found positive (throat). Both parents were negative for MRSA at that time, which suggests that the father was newly infected when his abscess developed and that he had not acquired the strain abroad. Also, spa typing indicated that the children carried different strains from that of the father and from each other (t286, t1434). Subsequent screening of family members for MRSA on several occasions found only the father to be repeatedly positive.Of note, the men's strain (ST398, t034) carried the two genes that express the toxin PVL, which is unusual in ST398, though characteristic of CA-MRSA USA300, the dominant community strain in the US. The role that PVL plays is very controversial: Some research groups believe it is responsible for the rapid tissue destruction that can accompany USA300 infection (in penumonia and some soft-tissue infections, for instance), while others vociferously disagree.
The second patient, a 43-year-old male clerk, also previously healthy, sought medical attention during the summer of 2007 for a MRSA-infected elbow wound. Follow-up examination determined that he carried MRSA also in the perineum and in a chronic external otitis eczema. He was later hospitalized for a larger abscess that required surgical drainage. His family members reported no symptoms and were thus not screened for MRSA.
18 March 2009
More MRSA in meat, in Austria
There's a new publication out that I haven't been able to lay my hands on yet, except for the abstract. But here's what I know: A group from the Austrian Agency for Health and Food Safety and two Austrian national reference laboratories have published a paper saying that ST 398, the "pig strain" of MRSA that we have been talking about here for a year now, has surfaced in Austria in environmental samples, in humans and also in food — presumably meat, but the abstract doesn't say that.
The abstract in Wiener Klinischer Wochenshrift (Viennese weekly clinical review, if my college German is still with me) says:
The University of Minnesota (where, as you all know, I work part time for the excellent infectious-disease news site CIDRAP; please go) does not have electronic access to this journal, and ILL is slow. If anyone else has a copy and would like to share, I would be grateful.
The cite is: Springer, B. et al. Methicillin-resistant Staphylococcus aureus: A new zoonotic agent? Wien Klin Wochenschr. 2009 Feb;121(3-4):86-90. Abstract here.
The abstract in Wiener Klinischer Wochenshrift (Viennese weekly clinical review, if my college German is still with me) says:
...the emergence of ST398 is not just a Dutch problem, as reports on livestock colonization and human infections are appearing worldwide. In Austria, the ST398 lineage has been detected in dust samples from pig breeding facilities and in food samples. Since the first Austrian detection of this emerging lineage in 2006, 21 human isolates, partially associated with infections, have been observed. MRSA has to be regarded as a new emerging zoonotic agent and livestock may constitute a growing reservoir of the ST398 lineage.
The University of Minnesota (where, as you all know, I work part time for the excellent infectious-disease news site CIDRAP; please go) does not have electronic access to this journal, and ILL is slow. If anyone else has a copy and would like to share, I would be grateful.
The cite is: Springer, B. et al. Methicillin-resistant Staphylococcus aureus: A new zoonotic agent? Wien Klin Wochenschr. 2009 Feb;121(3-4):86-90. Abstract here.
12 March 2009
New York Times takes up "pig MRSA" ST398
Constant readers, I know that many of you are very interested in ST 398, the "pig strain" of MSRA that has caused both mild and life-threatening human infections in Europe and has been found in retail meat in Canada and on farms and in farmers here in the Midwest. So I just want to bring to your attention that New York Times columnist Nicholas Kristof takes up the topic today, in the first of two promised columns: Our Pigs, Our Food, Our Health.
In today's piece, he describes an apparent epidemic of skin and soft-tissue infections in a pig-farming area of Indiana that caught the attention of a local family physician, who subsequently died.
What we'd need to know, of course — and may never know, given that the investigation may have ended with the doctor's death — is what strain of MRSA those local folks had. They may have ST 398, picked up if they worked on farms, or if it migrated out of the farms via groundwater or dust or flies. Or they may have USA300, the human community-associated strain, which in some areas is astonishingly common — a fact that most people don't appreciate if they have heard only about the invasive child-death cases or the outbreaks in sports teams.
The full archive of posts on MRSA in animals is here and stories only about ST398 are here.
In today's piece, he describes an apparent epidemic of skin and soft-tissue infections in a pig-farming area of Indiana that caught the attention of a local family physician, who subsequently died.
What we'd need to know, of course — and may never know, given that the investigation may have ended with the doctor's death — is what strain of MRSA those local folks had. They may have ST 398, picked up if they worked on farms, or if it migrated out of the farms via groundwater or dust or flies. Or they may have USA300, the human community-associated strain, which in some areas is astonishingly common — a fact that most people don't appreciate if they have heard only about the invasive child-death cases or the outbreaks in sports teams.
The full archive of posts on MRSA in animals is here and stories only about ST398 are here.
MRSA and animals — an elephant, this time.
So, constant readers, I have wrestled another chapter to the ground — and thus have a few minutes' breathing space to talk about a story that some of you have asked about privately. I've been wondering whether to post on this, because the entire episode is in the book, and I don't want to scoop myself. But it's so interesting, and so sad, that it seems worthwhile.
This episode happened a year ago, and was reported at a couple of medical meetings last fall, but it is in the news now because it was written up last week in the CDC's Morbidity and Mortality Weekly Report or MMWR. (Which is the best-read magazine that you have never heard of. Hundreds of thousands of people all over the world read it every week for the latest in disease news. It's free. Go, already.)
So, the brief synopsis: In late January 2008, the San Diego Zoo's Wild Animal Park noticed that a baby African elephant, born in late November 2007, had broken out in pustules on her ear, neck, elbow and leg. Three of her caretakers had skin infections also. The zoo launched an investigation, assisted by a CDC Epidemic Intelligence Service officer who is assigned to California; they were concerned that the caretakers had unknowingly picked up a disease from the baby, who had been born early, was not thriving and was being intensively hand-reared by the zoo staff.
But in fact, it was more complicated than that. The pustules were MRSA, of course — but they were not ST 398, the animal strain that we have talked about so much here. Instead, they were USA300, the community-associated human strain that has zoomed to dominance all over the country. But there was no MRSA in the elephant herd, which the baby had not had contact with since late December. The reconstructed chain of transmission looked more like this: from an unknowingly colonized human to the baby elephant, who was medically fragile and had been isolated from her herd, and then from the elephant to the rest of the human "herd" who were caring for her. The strain involved was USA300, In the end, five human infections and three colonizations were laboratory-confirmed, and 15 other infections were suspected but not confirmed.
The humans recovered; most of their infections were so minor as to need no treatment, though three of them took oral antibiotics. The poor little elephant was not so lucky. She had multiple other illnesses, and she was euthanized on Feb. 4, 2008. The MRSA did not cause her death — by the time she died, the infection had resolved — but as one of the zoo staff told me, "It certainly didn't help."
So what does this tell us? Well, for zoo personnel, it tells them what to do for next time: More complete infection control especially around vulnerable animals. For microbiologists, it's an expansion of MRSA's range: No one had ever seen it in an elephant before.
For animal owners, it's a warning and reminder. We've known for a while that community strains can transiently colonize pets, staying in the animal's nose or elsewhere on the body just long enough to reinfect a human — in fact, an emerging piece of advice for physicians dealing with recurrent MRSA in families is, "Check the dogs and cats, too."
And for the rest of us, it suggests, one more time, how extremely adaptive and inventive MRSA is, and that we should never underestimate its ability to surprise.
This episode happened a year ago, and was reported at a couple of medical meetings last fall, but it is in the news now because it was written up last week in the CDC's Morbidity and Mortality Weekly Report or MMWR. (Which is the best-read magazine that you have never heard of. Hundreds of thousands of people all over the world read it every week for the latest in disease news. It's free. Go, already.)
So, the brief synopsis: In late January 2008, the San Diego Zoo's Wild Animal Park noticed that a baby African elephant, born in late November 2007, had broken out in pustules on her ear, neck, elbow and leg. Three of her caretakers had skin infections also. The zoo launched an investigation, assisted by a CDC Epidemic Intelligence Service officer who is assigned to California; they were concerned that the caretakers had unknowingly picked up a disease from the baby, who had been born early, was not thriving and was being intensively hand-reared by the zoo staff.
But in fact, it was more complicated than that. The pustules were MRSA, of course — but they were not ST 398, the animal strain that we have talked about so much here. Instead, they were USA300, the community-associated human strain that has zoomed to dominance all over the country. But there was no MRSA in the elephant herd, which the baby had not had contact with since late December. The reconstructed chain of transmission looked more like this: from an unknowingly colonized human to the baby elephant, who was medically fragile and had been isolated from her herd, and then from the elephant to the rest of the human "herd" who were caring for her. The strain involved was USA300, In the end, five human infections and three colonizations were laboratory-confirmed, and 15 other infections were suspected but not confirmed.
The humans recovered; most of their infections were so minor as to need no treatment, though three of them took oral antibiotics. The poor little elephant was not so lucky. She had multiple other illnesses, and she was euthanized on Feb. 4, 2008. The MRSA did not cause her death — by the time she died, the infection had resolved — but as one of the zoo staff told me, "It certainly didn't help."
So what does this tell us? Well, for zoo personnel, it tells them what to do for next time: More complete infection control especially around vulnerable animals. For microbiologists, it's an expansion of MRSA's range: No one had ever seen it in an elephant before.
For animal owners, it's a warning and reminder. We've known for a while that community strains can transiently colonize pets, staying in the animal's nose or elsewhere on the body just long enough to reinfect a human — in fact, an emerging piece of advice for physicians dealing with recurrent MRSA in families is, "Check the dogs and cats, too."
And for the rest of us, it suggests, one more time, how extremely adaptive and inventive MRSA is, and that we should never underestimate its ability to surprise.
10 March 2009
Resistant bacteria on health care workers' phones
Here's some of the news that I mentioned Friday - no, I'm not hoarding, I'm just desperately behind on some writing (and falling further down the curve all the time, but thanks for the concern).
A team from Ondokuz Mayis University in Turkey, publishing in the open-access journal Annals of Clinical Microbiology and Antimicrobials, looked beyond the concern over health care workers' hands being clean, and decided to interrogate what those workers hold in their possibly-not-clean hands. They swabbed and tested the hands of 200 health care workers ("15 senior, 79 assistant doctors, 38 nurses and 68 healthcare staff "), and 200 phones. Their results:
The health care workers were certainly not infection-control outlaws: They washed their hands regularly. But only 10% of them had ever thought to clean their phones — which are held by the mouth and nose, a prime site for staph colonization, and go with them everywhere in the hospital, including to the OR and the ICU. (The paper doesn't make clear whether the phones in question are hospital-supplied, with potentially many users, or personal, with one user, but going from hospital to home and back again.)
So: We've talked in the past about the many challenges of infection control in hospitals — all the many, tiny details in multi-person, highly technological health care that can trip up even well-intended infection control. (Remember the sinks?) Here's just one more example of the unfathomable complexity of the journey of attempting to get to zero in healthcare-associated infections — a place, of course, where we all want to be.
The cite is: Ulger, F., Esen, S., Dilek, A. et al. Are we aware how contaminated our mobile phones are with nosocomial pathogens? Annals of Clinical Microbiology and Antimicrobials 2009, 8:7doi:10.1186/1476-0711-8-7
A team from Ondokuz Mayis University in Turkey, publishing in the open-access journal Annals of Clinical Microbiology and Antimicrobials, looked beyond the concern over health care workers' hands being clean, and decided to interrogate what those workers hold in their possibly-not-clean hands. They swabbed and tested the hands of 200 health care workers ("15 senior, 79 assistant doctors, 38 nurses and 68 healthcare staff "), and 200 phones. Their results:
- 94.5% of phones colonized with bacteria
- 49% of the phones grew one bacteria
- 34% grew two species, 11.5% three or more
- 50 of the phone and 53 health care workes carried S. aureus (approximately 25%)
- 52% of the S. aureus strains on phones were MRSA
- 37.7% of the S. aureus strains on hands were MRSA.
The health care workers were certainly not infection-control outlaws: They washed their hands regularly. But only 10% of them had ever thought to clean their phones — which are held by the mouth and nose, a prime site for staph colonization, and go with them everywhere in the hospital, including to the OR and the ICU. (The paper doesn't make clear whether the phones in question are hospital-supplied, with potentially many users, or personal, with one user, but going from hospital to home and back again.)
So: We've talked in the past about the many challenges of infection control in hospitals — all the many, tiny details in multi-person, highly technological health care that can trip up even well-intended infection control. (Remember the sinks?) Here's just one more example of the unfathomable complexity of the journey of attempting to get to zero in healthcare-associated infections — a place, of course, where we all want to be.
The cite is: Ulger, F., Esen, S., Dilek, A. et al. Are we aware how contaminated our mobile phones are with nosocomial pathogens? Annals of Clinical Microbiology and Antimicrobials 2009, 8:7doi:10.1186/1476-0711-8-7
06 March 2009
A little public-health humor
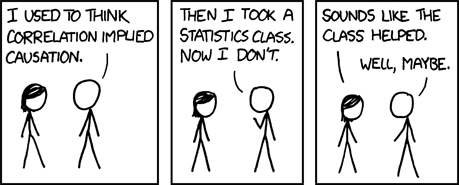
Constant readers - lots of new news happening, and blogposts coming. While I organize it, here's a strip from one of my favorite webcomics, XKCD.com.
04 March 2009
Industrial farming, bacterial spread 2 - or: Flies. Ick.
There's a brand-new paper in the journal Science of the Total Environment that has some unnerving things to say about the link between very large scale farming, use of antibiotics in food animals, development of resistant organisms, and transmittal out into the larger environment.
Via flies.
Not to be unscientific, but: Ick.
A team from the Bloomberg School of Public Health at Johns Hopkins (who have done a number of studies on the spread of antibiotic-resistant organisms from farms to the outside world) decided to test the links in a chain of hypothesis that goes like this:
And the findings were: Oh, lots and lots. Litter piles at all three farms contained resistant organisms — E. faecium, E. faecalis and our particular interest, Staphylococcus (multiple species, including three strains of S. aureus) — throughout the 120-day study period. All 8 fly traps did as well. All of the litter contained enterococci and staph strains that were resistant to 3 or more antibiotic classes. Seven of the 8 fly traps yielded multi-drug resistant enterococci, and 3 yielded multi-drug resistant staph. The resistance factors identified were for drugs that the FDA classifies as "critically or highly important" to human medicine: "penicillin, tetracyclines, macrolides, lincosamides, aminoglycosides and streptogramins." Oh, and the fly species captured in the traps had an average range of 2 miles.
Of note, among the isolates discovered was one staphylococcus with high-level resistance to vancomycin.
The authors say:
The cite is: Graham JP et al., Antibiotic resistant enterococci and staphylococci isolated from flies collected near confined poultry feeding operations, Sci Total Environ (2009), doi:10.1016/j.scitotenv.2008.11.056. The ahead-of-print abstract is here.
Via flies.
Not to be unscientific, but: Ick.
A team from the Bloomberg School of Public Health at Johns Hopkins (who have done a number of studies on the spread of antibiotic-resistant organisms from farms to the outside world) decided to test the links in a chain of hypothesis that goes like this:
- Antibiotics are used in large amounts in poultry production.
- Antibiotic-resistant organisms are produced within the birds.
- Antibiotic-resistant organisms leave the batteries via poultry litter ("excreta, feathers, spilled feed, bedding material, soil and dead birds").
- Poultry litter is stored in open sheds until it can be used as a soil amendment.
- Flies have unrestricted access to poultry litter.
And the findings were: Oh, lots and lots. Litter piles at all three farms contained resistant organisms — E. faecium, E. faecalis and our particular interest, Staphylococcus (multiple species, including three strains of S. aureus) — throughout the 120-day study period. All 8 fly traps did as well. All of the litter contained enterococci and staph strains that were resistant to 3 or more antibiotic classes. Seven of the 8 fly traps yielded multi-drug resistant enterococci, and 3 yielded multi-drug resistant staph. The resistance factors identified were for drugs that the FDA classifies as "critically or highly important" to human medicine: "penicillin, tetracyclines, macrolides, lincosamides, aminoglycosides and streptogramins." Oh, and the fly species captured in the traps had an average range of 2 miles.
Of note, among the isolates discovered was one staphylococcus with high-level resistance to vancomycin.
The authors say:
This study strongly suggests that flies in intensive poultry production areas, such as the Delmarva Peninsula, can disperse antibiotic resistant bacteria in their digestive tracts and on their exterior surfaces. Dispersion of resistant bacteria from poultry farms by flies could contribute to human exposures, although at present it is difficult to quantify the contribution of flies. Flies may also transfer bacteria from fields amended with poultry waste.
The cite is: Graham JP et al., Antibiotic resistant enterococci and staphylococci isolated from flies collected near confined poultry feeding operations, Sci Total Environ (2009), doi:10.1016/j.scitotenv.2008.11.056. The ahead-of-print abstract is here.
Subscribe to:
Comments (Atom)